subscapularis tendon tear recovery time
 Subscapularis Tendon Rupture - Everything You Need To Know - Dr. Nabil Ebraheim - YouTube
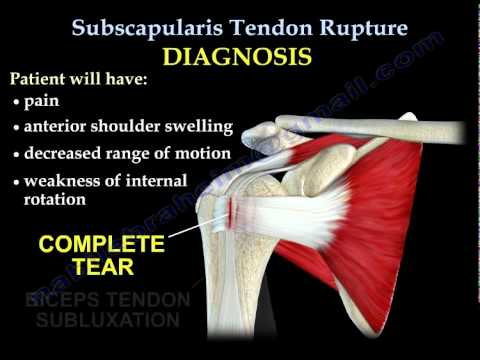
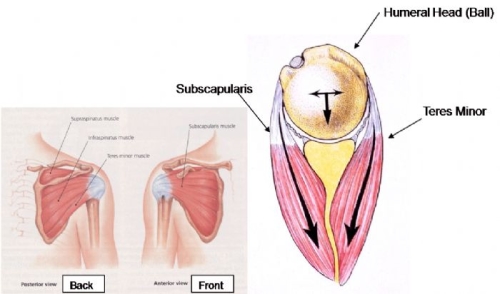
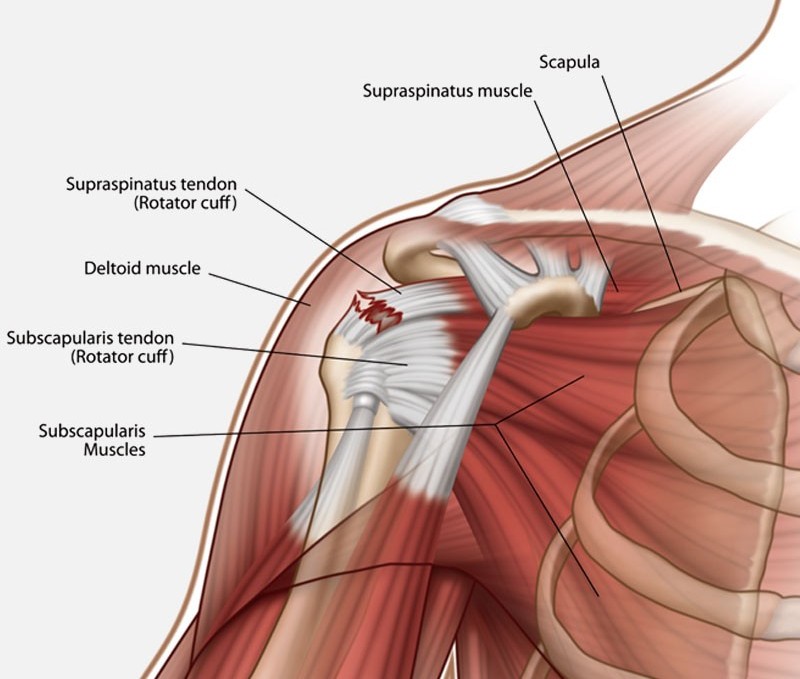
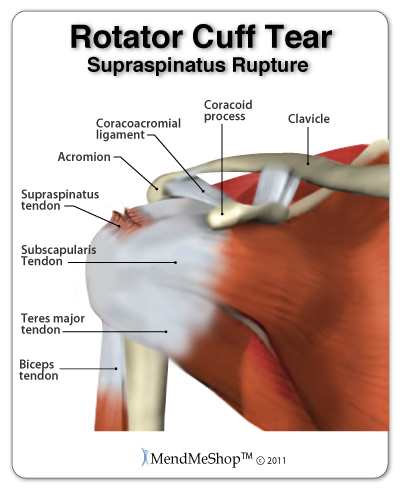
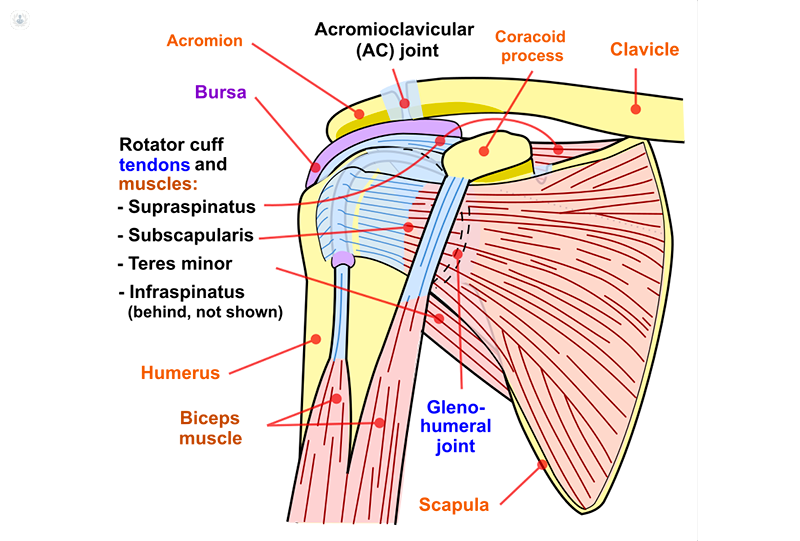
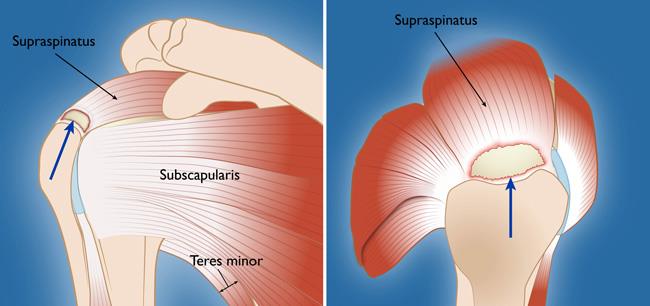
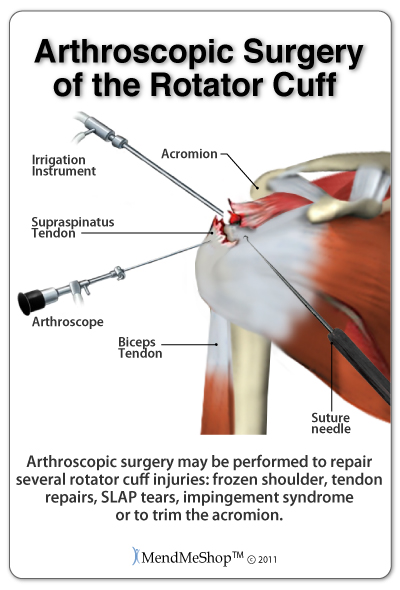
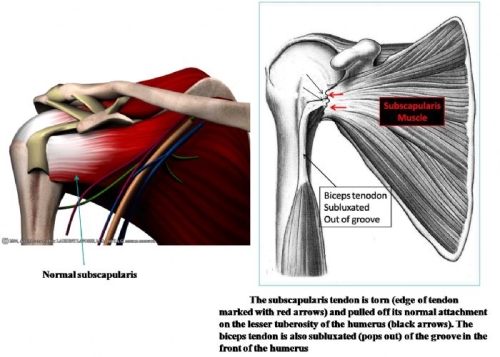
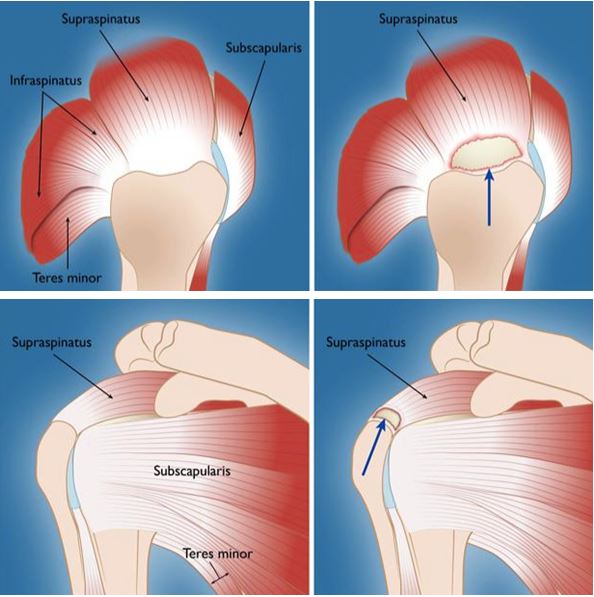
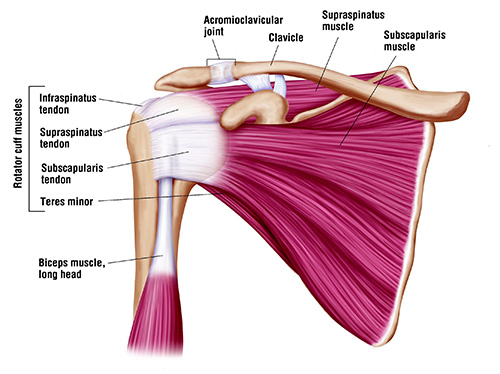
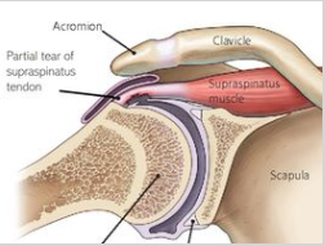
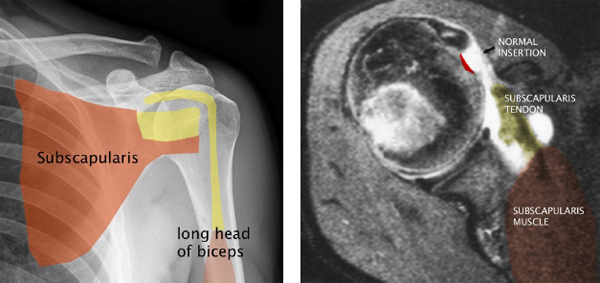
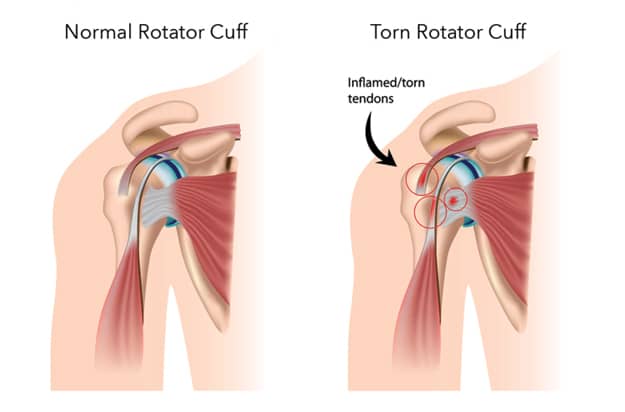
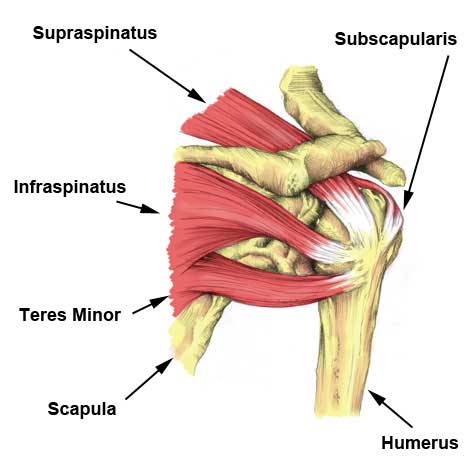
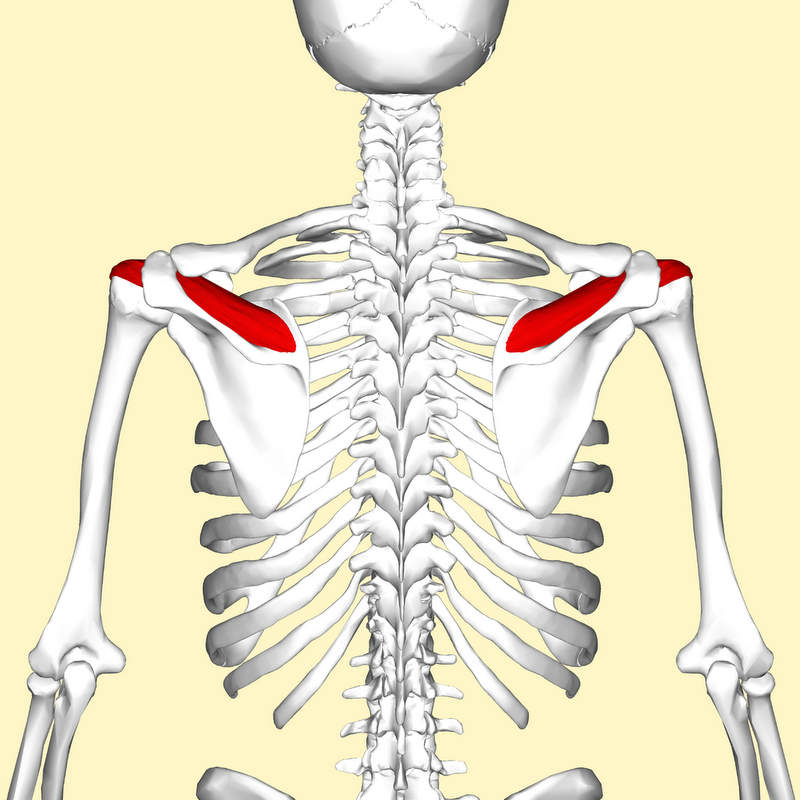
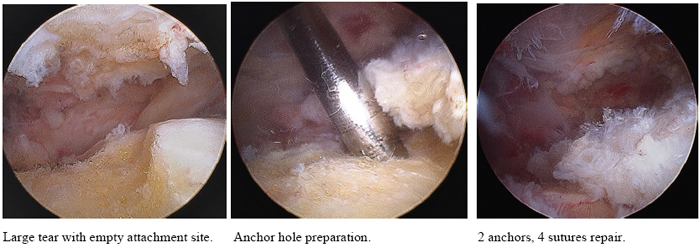
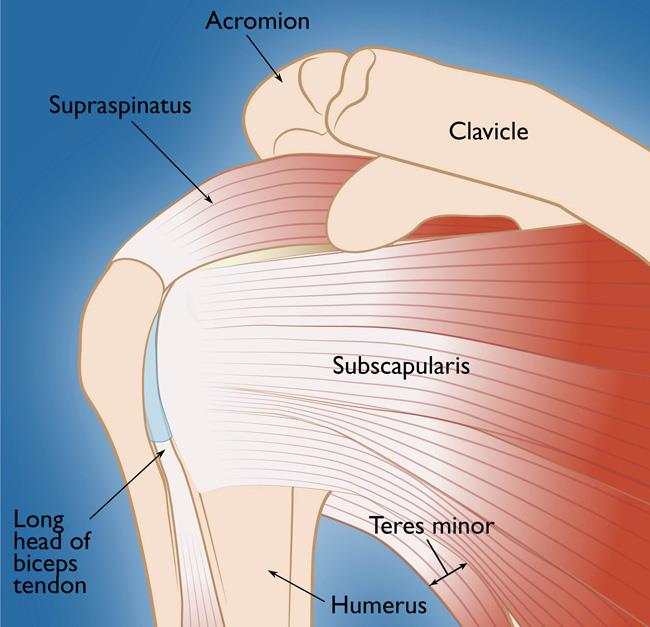
Subscapularis Tendon Rupture - Everything You Need To Know - Dr. Nabil Ebraheim - YouTubeWarning: The NCBI website requires JavaScript to operate. FOLLOW US SUBSCAPULARIS TENDON REPAIRBurak Altintas1Steadman Philippon Research Institute, Vail, CO, USA3The Steadman Clinic, 181 West Meadow Drive, Suite 400, Vail, CO. 81657Helen Bradley2 Howard Head Sports Medicine, Vail, CO, USACatherine Logan1Steadman Philippon Research Institute, Vail, CO, USA3The Steadman Clinic, 181 West Meadow Drive, Suite 400, Vail, CO. 81657 Brooke Delvecchio2 Howard Head Sports Medicine, Vail, CO, USANicole Anderson1Steadman Philippon Research Institute, Vail, CO, USAPeter J. Millett1Steadman Philippon Research Institute, Vail, CO, USA3The Steadman Clinic, 181 West Meadow Drive, Suite 400, Vail, CO. 81657AbstractThe inner tears of the tendon are less common than the main consequences. Mild fraying involving the upper third of the tendon can be treated non-operatory; however, the most substantive tears usually require repair in cases of pain or functional deterioration. Given the importance of the subscapular tendon to maintain the stability of the glenohumeral joint and perform the internal rotation of the arm, surgery can be recommended with emphasis on repair to eliminate pain and restore strength. Postoperative rehabilitation through gradual progression is used to avoid premature stress in the healing tissue while allowing early return to daily activities. The purpose of this clinical commentary is to provide a evidence-based description of postoperative rehabilitation after repairing the SSC tendon with guidance for safe and effective return to activity and sports. Test Level5INTRODUCTION Subscapularis tendon (SSC) forms the previous section of the rotating cuff (RC) and its muscle is the largest and most powerful rotating cuff muscle. The upper 60% of the insertion is tendentious and the lower 40% consists of muscle. The SSC is one of the most important previous stabilizers of the glenohumeral joint. It balances the force pair in the horizontal and frontal planes. In addition, the SSC works primarily as an internal rotator, while its superior fibers help to hijack the arm and its lower fibers help to adduct it. The tears of the SSC tendon are less common than the tears of the remaining rotating cuff tendons. The prevalence of CFS tears was reported to range from 31.4 to 37% in patients under arthroscopic rotating cuff surgery. Most of the tears of subscapular tendons are degenerative in origin, however some result from trauma following an earlier dislocation of the shoulder or more commonly after the force of violent external rotation, as in a car accident. The tear and dislocation of the long head of the biceps is very common in conjunction with the rupture of the subscapular tendon due to the loss of its medial limitation as the tears of the pulley. The classification of the lesions of the SSC tendon has been described by Fox and Romeo along with Lafosse et al. Surgical repair is usually advocated for full-size tendon lesions. The size of the tear, the quality of the tendon tissue, the degeneration of muscle fat and the chronicle of the condition can have drastic effects on the result of these repairs. In addition, subcoracoid impingement can cause a "reel thread effect" on the SSC tendon and contribute to the pathogenesis of SSC tears. Therefore, the superior author performs a subcorcoid decompression simultaneously with the SSC repair. The literature focused on rehabilitation after repairs of the SSC tendon with attention to the return to sport is limited. This document will examine the recommended rehabilitation guidelines after repairing the full-size SSC tears 1/3 in front of the extensive tears of SSC to direct muscle insertion. The purpose of this clinical commentary is to provide a evidence-based description of postoperative rehabilitation after repairing the SSC tendon with guidance for safe and effective return to activity and sports. Biomechanics As the most powerful rotating cuff muscle, SSC contributes to 53% of the time of the wives. The strength generating capacity is equal to that of the other three combined muscles. A breakdown or breakup of the subscapularis muscle may manifest as pain, weakness with internal rotation (IR) and increase the passive movement with external rotation (ER) or previous glenohumeral instability. The upper and upper portions of the SSC were shown with significantly higher rigidity compared to the lower region both in the hanging arm and in 60 ° of kidnapping. It was concluded that increased stiffness and a maximum load in the upper region of the tendon can explain the extent of tears of rotary cuff in the SSC tendon. Clinical examination The integrity of SSC can be evaluated with the pressure of the belly, the take-off, the modified take-off, the bear tests and the belly out of signal. The abdominal pressure test was described by Gerber et al. and is performed with the arm on the side with the elbow flexed to 90 ° and the palm held against the stomach.Then the patient is asked to push his palm to his abdomen while the examiner throws in the opposite direction. A positive test is noted for the patient's inability to resist or for compensation through the bending of the wrist and/or the extension of the arm. In addition, you can see a combination of extension and shoulder attachment due to compensation through latissimus and pectoralis. The take-off test is performed with the back surface of the hand placed on the lumbar column. The patient is asked to turn the shoulder internally by lifting the hand of the spine. A positive test is denoted by inability to lift the dorsum of the hand or for compensation through the elbow and/or the extension of the shoulder. The modified disassembly test is performed with the patient's arm rotated and extended on the back with the hand of 5 to 10 cm of the skin, followed by the release of the arm. The test is considered positive when the hand lands on the back. This is also considered the IR lap sign. The bear hunt test uses resisted IR while the palm is held on the opposite shoulder while the elbow is held in a maximum previous translation position. With the belly signal turned off, the patient's arm passively enters into flexion and maximum IR with 90 ° of bending. The sign of the belly occurs if the patient cannot maintain this position and flex the wrist or a lag occurs. Surgical management The repair of the broken SSC tendon involves adjustment to the anatomical footprint in the lower tuberosity with suture anchors, which can be done arthroscopically or through an open surgical approach. The technique used by the main author has been previously published by Katthagen et al. All procedures are performed with the patient in a beach chair position under general anesthesia with an interscalane nervous block. Following the standard diagnostic arthroscopy and confirming the size of the SSC tear, the decompression of subcorcoid soft tissue is performed along with the release of any adhesion around the broken tendon. For partial tears, a technique of repair is preferred without knots. To make this easier, a spinal needle is percutaneously placed through the tear and a polydioxanone suture (PDS) is released through a higher anterior portal. Then a suture tape (FiberTape, Arthrex) is passed through the tear. After preparing the SSC anatomical footprint with a shave to create a hemorrhage and tapping bone bed, the suture tape is passed through a bioabsorbable anchor (4.75 Bio SwiveLock, Arthrex). The anchor is then inserted into the lower tuberosity and the tendon is secured back to the bone. In SSC tears of all kinds involving tendentious portion, the superior author prefers to perform an arthroscopic repair in a dual-leaf technique, linked, without knots, broken (SpeedBridge, Arthrex, Naples, FL). The SSC is visualized arthroscopically after a subcorcoid decompression. After the mobilization of the tendon tube and the debridation of the tendon footprint in the humerus to a bleeding surface, the average anchors are placed approximately 1 mm of the joint margin. The suture tapes are passed through the SSC tendon. The SSC tendon is compressed on the footprint and the side anchors are insured. The arm is taken through a range of motion to confirm that the SSC is safe and stable, and has a proper tension. For massive tears that involve direct muscle insertion or chronic retracted tears, an open, deltopectoral approach can be used. In all cases of SSC tear and when the biceps pulley is interrupted, a biceps theorosis is performed. Biceps are released arthroscopically and a biceps subpectoral tenodesis is performed with an interference screw. The concomitant pathology of the long head of the biceps (LHB) is common in the lesions of the SSC tendon. Tahal et al. showed that sub-pectoral bicep thenodesis is an excellent treatment option for active patients with LHB tenosinovitis and chronic anterior shoulder pain, resulting in a decrease in pain, a better function, a high satisfaction and a better quality of life. This is our preferred treatment option for LHB pathology. Immediately after the operation, the shoulder is immobilized in a cage. passive ROM early starts with a limitation of 30° ER. Given that a concomitant LHB tenodesis is performed when repairing the SSC, resisted elbow bending should be avoided for 6 weeks. In addition, resisted supposition should also be avoided to minimize general stress to biceps. Clinical result Seppel et al. investigated the long-term results of the arthroscopic repair of the isolated tears of the SSC, reporting significant clinical improvements and the integrity of the durable tendon. However, SSC strength has been reduced in the long term, 88.2% of patients were "very satisfied" or "satisfied" with their results. In a previous study, Adams and colleagues reported results of SSC arthroscopic repairs in an average follow-up of five years, finding 80% (32 out of 40) of patients had a good or excellent result after an arthroscopic STR. Recently, Katthagen et al. reviewed the results of the older author's patient (PJM) and showed improved results with high patient satisfaction following the arthroscopic repair of the third upper CFS tear in 31 patients with an average follow-up of 4.1 years. They reported more favorable outcomes following repair of full-thickness upper third SSC tears compared with high grade partial-thickness upper third SSC tears. REHABILITATION CHARTERA successful outcome after SSC repair surgery is a painless and stable shoulder that has sufficient mobility, stability and strength for the desired level of activity and participation of a patient. Postoperative rehabilitation is adapted to the individual according to criteria and functional progression, taking into account the healing timelines, the achievement of specific clinical goals and in conjunction with the recommendations of the sender physician. The healing phases include the inflammatory phase, the proliferation phase (reparation) and the remodeling phase. The overall objective of rehabilitation focuses on the principle of the gradual application of the shoulder-controlled tensions with consideration of the healing phases to optimize the patient's outcome. Literature to support the effectiveness of a specific rehabilitation protocol for SSC repair is limited. The rehabilitation after the repair of the SSC depends on the extent of the injury and will vary as to whether the repair implies a total break of the 1/3 superior of the tendon against the repair of the entire tendon until direct muscle insertion. Clinicalians, surgeons and physical therapists must have a functional knowledge of the anatomy and kinematics of the shoulder complex, underlying pathophysiology, tendon healing principles and specific attributes and limitations of certain treatment interventions and should select treatment strategies accordingly to achieve an optimal result. It is necessary to unify time-based and performance-based criteria, with milestones for each of them that are met before progression to the next phase. Millett et al. highlighted the importance of an evaluation-based rehabilitation protocol that takes into account not only healing times but also the achievement of specific clinical objectives., Criteria are proposed to move forward in each phase of rehabilitation by merging time-based and performance-based principles. This respects the biology and temporal aspects of healing, while at the same time requires functional objectives to be met before progression to the next phase of rehabilitation. This program allows the patient to reach a strong base on mobility, strength and strength before returning to unrestricted activity or sports performance. Suggested guidelines for rehabilitation were developed after repairing full-size tears of 1/3 and extensive SSCs based on current literature, best available tests and professional experience. This should provide doctors who treat these injuries with guidelines to improve rehabilitation after surgery. The rehabilitation programme is divided into five phases. The underlying pathology, the integrity of the repair and biology of healing along with the desired level of activity will determine the progression rate through the five phases. Phase I is the maximum protection phase involving immobilization with only passive exercises that minimize loads through repair. The muscle resistance phase, Phase II, consists of the introduction of active exercises, which gradually apply burden to repair and begin to transfer burdens back to healing tissues. Phase III focuses on muscle strength, incorporating resistant exercises to continue applying tissue-controlled stress. If the individual does not require advanced movements or power for his or her daily life (ADL), occupational or sporting preferences, meeting phase III objectives could result in the completion of rehabilitation. If the individual has high physical requirements of his or her work or sport he needs to progress through the power Phase IV and/or Phase V return to sport may be necessary. PHASE I: PROTECTION PHASE The objectives of this phase of rehabilitation are to maximize surgical reconstruction, optimize the environment for tissue healing, reduce pain and inflammation, restore passive mobility to minimize stiffness (being aware of not exceeding the limits of ER), and the reduced ADL pain with the use of a fold. These objectives should be addressed without causing inappropriate stress to healing structures. Good communication between the physical therapist, the patient and the surgeon is essential at this stage and helps to run the rehabilitation course. Patient-related factors, such as previous surgery, smoking and comorbidities, have a negative impact on tendon healing, rehabilitation and ultimately on clinical outcomes. Each variable should be considered when formulating a postoperative therapy plan, which should be adapted to each individual case. The education of patients to transmit the rationality of the outlined rehabilitation protocol and the importance of protecting the healing tissues from excessive stress is essential to ensuring compliance. Protection To reduce the tension in repair, the shoulder is protected for four weeks. This is achieved using an abyss during the day and night. The authors suggest protecting the arm in light abduction to promote optimal blood flow and minimize the tension for repair. Patients are allowed to have waist-level activity in the sling (i.e., keyboard) as tolerated. Gurney et al. evaluated the electromyographic activity (EMG) of the shoulder during common tasks such as ambulation, donating/doffing to sling and other movements. The authors showed that rehabilitation tasks such as pendulum exercises, passive range of movement performed by a physical therapist, and self-ranged movement with a dowel showed low EMG activity, while the ambulation without an aguijón, donating / making a sting and pulley in the sagittal and scapular plane showed greater activity. These findings indicate that caution is needed after STR when donated/ made a sling and highlights the importance of using sling during ambulation. Cryotherapy Continuous cryotherapy has been shown to cause a significant reduction in the temperatures of glynohumeral joint and sub-bacromial space on the shoulder in variable times during the first 23 postoperative hours. Cryptotherapy should be used during this phase to control pain, decrease inflammation and muscle spasm, suppress inflammatory response and improve sleep patterns. Motion RangeActive hands, wrist and elbow range of movement should be part of a domestic exercise program. The authors encourage early passive ROM exercises for glynohumeral joint. Keener et al. could not show an apparent advantage or disadvantage of the early passive range of movement (PROM) compared to immobilization in a randomized prospective trial after repairing the arthroscopic rotating cuff. It has been shown that the passive continuous movement properly applied (in the knee and elbow) during the first two stages of stiffness (sangrade and edema) after surgery acts to pump blood and fluid edema away from the joint and periarticular tissues. This allows the normal compliance of the periarticular soft tissue. Early ROM prevents adherence and when repair is safe and the quality of the tissue is good, the PROM is allowed early. ER is usually limited to avoiding undue burden in the incipient SSC repair. Immediately after surgery, repair depends on the mechanical strength of sutures and anchors. Therefore, the active movement of the shoulder joint at this time would overly emphasize healing tissues. In these cases, a gradual progression of PROM is recommended for four weeks. However, with the shoulder to 0 ° rapture, the passive glynohumeral ER past 30 ° emphasizes the previous capsule, as well as the SSC muscle and is not recommended after repairing a SSC tendon tear for three weeks. For a massive tear, with very poor quality tissue or undue strain on repair, the authors sometimes limit ER to neutral for several weeks to avoid the stress of repair. After repairing the SSC, passive internal rotation should be limited to the belt line for the first four weeks. Scapula During the first two weeks after repairing a large full thickness tear of SSC, excessive scapular mobility can emphasize repair and must be avoided. After two weeks or initially after superior repairs 1/3 SSC, scapular mobility exercises can be incorporated. The normal active scapular movement (protraction, retraction, elevation and depression) helps facilitate early neuromuscular control of the escapula. The lateral scapular clock exercise is a great starting point for this with progression to sit down or stand with the sting on. IsometricsTo protect the repair of the skiing or compressive forces, is not to perform isometric exercises during the weeks 0-3 after repairing extensive SSC tears and weeks 0-2 after the superior repair 1/3 SSC. After this time you can start isometric exercises of the muscles surrounding the shoulder belt. These should be submaximums and non-painting, with the shoulder in a neutral position. The rhythmic stabilization, which implies a gentle manual resistance to the proximal forearm using oscillating disturbance in a neutral shoulder position, is suitable to facilitate the low contraction of the scapular and rotating cuff musculature and can be beneficial for early neuromuscular re-education. Manual therapy Manual therapy during this phase should consist of soft tissue techniques and PROM. The soft tissue techniques initially include lymphatic drainage to help with the reduction of swelling and subsequently include upper-quarter miodal liberation techniques and portal scarc mobilization techniques. Glenohumeral's mobility is not assessed due to curative structures and post-surgical precautions, as the previous humeral rigid could put excessive strain on the repaired SSC. Cynetic Chain Exercises Aborting the early kinetic chain in rehabilitation will benefit the patient in the long term, so basic breathing exercises must be incorporated into this stage of rehabilitation. Basic exercises in a hook position with the sling in, with focus on the lower extremity movement will ensure that the surgical reconstruction is safe and not stressed. Stationary recumbent bicycle should be encouraged to keep the patient from cardiovascular condition, increase blood flow to healing tissues and for mental health benefits. The approach to progress in the next phase of rehabilitation is described in the table. The questionnaire on the disability of the weapon, shoulder and hand (DASH) can also be used as a criterion for progression. In addition to this, it is important to work with the individual surgeon to obtain his preferred time frames for progression and understand his rationality in deciding the ROM restrictions. Table 1 Criteria for Progression of Tendon Algorithm. PHASE II. MUSCULAR FINURITY The main objectives of this phase are careful progression to full active ROM (AROM), improvement of muscle resistance and neuromuscular control of the shoulder complex. In addition, the normal use of the limb involved for ADLs must be achieved at the end of this phase with the exception that they are not lifted, moved quickly or repetitive activities are carried out. During this phase the sling and ROM progressed to include ROM (AAROM) and AROM active assisted. PROM and light stretching should continue as necessary until full PROM is reached. If deficits remain, low loads, long-term stretching and joint mobilization can be used at 5-6 weeks after the operation. Isotonic exercises should focus on high repetitions with low or no resistance. Gravity alone for resistance is often enough at this time. Individuals who follow repairs of the smaller SSC's upper 1/3 tears normally move to this phase a week before those who have larger or more extensive tears due to the previous period to start the AROM. AAROM starts a week before AROM begins, as it is important to gradually apply the load without overloading the healing structures during this phase. Equipment like a foam roller and ball stability can be used to allow the patient to advance AAROM, as maintaining the low muscle activation of the SSC after repair is important. The previous literature has used EMG studies to guide postoperative rehabilitation progression in the RC after surgery with 15% MVIC considered as a higher limit of a safe load range during the exercises in the initial stages of the movement after repair. The table slides, pulley-assisted lift, roast row, wall-assisted ER have proven to have a 15% or less MVIC. Patients may have significant deficits in ER mobility due to postoperative restrictions; the use of a bar is encouraged to progress ER AAROM in supine. Once the patient displays effective isometric muscle contraction, as well as a fair muscle activation with AAROM, AROM initiation can begin. ROM can be made in supine, lateral or prone positions to reduce the effects of gravity, progressing to a permanent position while improving resistance. For example, the progression of the shoulder abduction would begin with supine, AAROM slide board with a bar (), to the abduction of lateral shoulders that would add rhythmic stabilization to help with neuromuscular control (), advance to T (horizontal abduction) () and permanent abduction/adduction against a wall with focus on scapular control. Motion abduction range with active supine help in the slide table with bar. a, b) Side sequester c) Ritmic stabilization. Proprietary horizontal aggregation (T's). It is vital to incorporate ROM exercises that improve scapular control during this phase. A synchronized contribution of scapular musculature is essential for optimal position, stability and operation of the shoulder complex. The upper muscles (UT), medium (MT) and lower rag (LT) and the former serrato muscle are the largest contributors to scapular stability and mobility. It is clinically important to improve LT/UT and MT/UT activation relationships as a dominant UT has been linked to shoulder pathologies due to contributions of poor postures and muscle imbalances. Private exercises that have been shown through EMG studies to accentuate periescapular control by minimizing the muscle activation UT are lateral ER, lateral front bending, prone horizontal rapture with ER, prone bending and prone extension.– These activate the key scapular muscles stabilizing without putting high demands on the shoulder joint. Functional shoulder stability is achieved through passive and active mechanisms. The passive mechanisms include the geometric configuration of the joint and the integrated functions of the joint capsule, ligaments and the glenoiding labrum. Active mechanisms include the dynamic stabilization of the surrounding musculature and the inervation of those muscles, in particular the musculature of the rotating cuff. In addition, dynamic stabilizers provide stability through an active mechanism called neuromuscular control. Dynamic stability is achieved through proprioceptive and kinstatic consciousness and efficient muscle activity, which is achieved through the efficiency of several shoulder muscle strength couples. SSC and pectoralis musculature work together with external rotators to establish the internal/external rotating force couple that works according to the deltoid. The dynamic glenohumeral stability is achieved by these couples of strength through joint compression, ligamentary tension and competent neuromuscular control. An essential objective of therapeutic exercise should be directed towards improving neuromuscular control and thus improving the dynamic functional stability of the glynohumeral joint. As the ROM objectives are met, the rehabilitation approach can change to neuromuscular reeducation. Neuromuscular training should provide a gradual increase in muscle demand to protect healing structures and also prevent abnormal motion patterns from developing. Ritmic stabilization can be started at various angles and diagonal propulsive neuromuscular facilitation guidelines to help gain stability and control in functional patterns. Open-chain scapular exercises, such as the puncture supine serratus/plus can help establish appropriate scapular-toracic strength couples and improve neuromuscular resistance with AROM. Loaded closed chain exercises are not appropriate during this phase as they can create too much joint stress and negatively affect surgical repair. The closed kinetic chain scapular exercises downloaded, such as wall slides () or wall more, can be cautiously started at this time. The closed chain scapular exercises should be started in Phase III to allow sufficient time to develop proper dynamic stability before starting the compressive forces of the glenohumeral joint. Wall lenses with foam roller (No charge). This phase of rehabilitation may potentially require a significant amount of time to properly retrain the rotary cuff and periescapular musculature. Before moving forward in Phase III of rehabilitation, the patient needs to achieve adequate PROM, as well as the unpainted shoulder and the escapulothoracic AROM (see Table ). PHASE III: STRENGTH MUSCULAR Following the establishment of good activation and muscle resistance in Phase II, the main objective of Phase III is to improve strength by increasing resistance and reducing repetitions, to advance muscle resistance and dynamic stability exercises. This can be done through a periodization format to load repair and stimulate healthy remodeling. It is recommended that the initial strengthening not begin before 6 weeks after the operation and that the advanced strengthening is delayed until 10 weeks after the operation. Iannotti et al. could be shown in a prospective study of re-tear images occurred mainly between six and twenty-six weeks after repairing arthroscopic rotating cuffs, thus underlining the importance of this recovery phase. Since this is a progression based on criteria, people should not begin this phase until the objectives of phase II are met, therefore there can be a significant variability among individuals who begin to strengthen themselves. A strengthening program is used for the entire shoulder belt, with focus on the rotating sleeve and periscapular musculature. Initially the unregistered exercises described in Phase II are implemented with the addition of resistance. Drums, elastic cords (), cable machines, barbeque weights and manual resistance including disruption can be added to these exercises to make them more challenging. The approach should be in controlled and eccentric concessions. The initial strengthening exercises must be chosen that have shown EMG activation of 21-50% MVIC. Specifically for the SSC this includes the assisted lifting of vertical bars, front bumps and RI to 0 ° abduction. Internal rotation in 45o with the elbow supported on the table with a sports cord. During the late strengthening phase, the activation of EMG of 50% MVIC can be started. These include IR to 45 ° rapture, ER to 0 ° and 90 ° rapture; dynamic hug; diagonal; IR to 90 ° rapture; low row, high row, resisted shoulder extension; resisted lifting/active bending. () dynamic hug with sports cord. The balance between the external and internal rotation force (ER/IR) is important for the normal glenohumeral joint function. In the literature, an adequate proportion of external-internal rotating muscle strength has been emphasized with a minimum of 65% and optimally between 66% and 75%., a greater EMG activity of the SSC has been reported with internal rotation to a 90 ° abduction (IR90) compared to the kidnapping of 0 ° (IR0). Previous studies have recommended SSC strengthening exercises in adduced positions; on the contrary Alizadehkhaiyat et al. found a significantly greater activation of SSC along with the low to moderate activation of pectoralis major, latissimus dorsi and major teres in IR90, indicating a preference for this exercise for selective activation SSC. This finding is online with Decker et al. which showed higher levels of pectoralis and latissimus dorsi activation in IR0 compared to IR90, and suggested that IR90 would be more beneficial to strengthen SSC due to the minimization of the contributions of larger muscle groups. Initially, closed-chain body weight exercises are performed as isometric or static exercises, which can be progressed to increase weight through the upper extremities. The advance of the wall to the table or to the quadruped position creates a gradual increase in the load and is excellent for scapular control. Some examples include the boost with a plus, which has demonstrated high EMG activity for SSC; and the upper quadruped extremity and the lower extremity reach, which also challenges basic stability. Place an unstable base under the upper extremities as a ball of stability or BOSU®, improves neuromuscular control at a level of reflection while the disturbance will challenge the proprioception and improves the sense of joint position. At the end of this phase, light impact activities can be included. It is important to perform force tests periodically throughout this phase to identify specific muscle deficits and focus the exercise prescription accordingly. Hand dynamometry (HHD) offers a precise means of evaluating muscle strength. Kokmeyer et al. promoted the use of an HHD to determine a lamb symmetry index (LSI). (Figure) This study suggested a resistance index of 90% or greater is a good reference objective, when evaluating the willingness of an athlete to return to the sport (RTS). The criteria for progressing Phase IV require the athlete to have an LSI of 80% or greater relative to ER/IR to be 70%. HHD tests isometric muscle resistance and should be used in several positions to test all rotating cuff muscles, specifically ER0, IR0, ER90, IR90, kidnapping and escaping at 90°. For clinical evaluation, both abdominal pressure and take-off tests are valid and specific to the SSC assessment. The abdominal pressure test was found to activate the upper SSC muscle significantly more than the take-off test, while the take-off test was found to pose a significantly higher challenge to the lower SSC muscle than the abdominal pressure test. In addition to the strength objectives, individuals must have ROM active on the counter-lateral side and achieve three of the five tasks described in the table. If the individual has occupational or athletic demands that require higher power or force movements, they will advance to Phase IV of the rehabilitation program. Otherwise, once these goals are reached, they can be released from therapy with a home exercise program. Handheld dynamometer test (HHD) – Press Belly. Manual dynamometer tests (HHD) – Internal rotation at 90 °. The main objectives of this phase are to incorporate speed, explosive strength and introduce biased motion patterns towards the specific sport or occupational demands of individuals. It is the role of the physical therapist to further develop and identify the patient's program. Repetition, speed and load can be varied in relation to the desired task, facilitating the processing of food forward. Pyometric exercises are an excellent and functional method for an individual to increase the power, strength and stability of the RC and the activation of the pericapular musculature. Pyometric exercises should focus on SSC muscle combined with trunk stabilization. Beginning with double pyometric exercises of upper extremity, such as clams to the ground, thrown up against a wall and side shots against a wall (). Progressing to monometric exercises of superior extremity unique as power, strength and capacity allow. These exercises can be performed with 90° of glynohumeral articular rapture that prepares the athlete for a return to the demands of the overhead function and has been shown to improve the IR/ER force and launch the performance after 8 weeks of training. During the rolling phase of the spear, the SSC eccentrically contracts to decelerate ER and protects the previous and lower structures of the glenohumeral joint. The acceleration phase is very explosive and requires the SSC to contract concentrically. Single-armed plyometric exercises include IR wall drip, IR shots against a trampoline and supine 90/90 IR balls using a light-handed medicine ball. A) Side launch against the wall with the ball of medicine (start) B) Side launch against the wall with the ball of medicine (finish). In this phase, closed chain exercises are performed to prepare the individual to return to sporting requirements. It has been shown that suspension training, such as the TRX® system, produces greater activation both in the upper arm muscles and in the previous trunk when a spike-based push is made in front of a soil thrust. To progress the weight beyond and increase the load through the shoulder complex, the feet can be suspended on the straps while a ground push is made. Moving to phase V of rehabilitation requires the athlete to have no pain, ROM deficiency or scapular dyskinesis. In the literature, a limited selection of functional tests has been identified to evaluate the preparation of an RTS athlete. The most appropriate, reflective test of the specific sports requirements of the athlete must be used and approved successfully before moving to Phase V. These tests include one-armed injection tip tests, upper extremity Y-Balance test (UEYBT), upper-end stability test of closed kinetic chain (CKCUEST) and wall-mounted plymmetrical medicine ball exercises. PHASE V: RETURN TO SPORT The aim of this phase is to successfully return the athlete to full sport participation without compensation, risk of rejudge or dysfunctional motion patterns. The load is moving towards normal levels of participation by increasing volume and intensity. It is recommended that specific clinical trials and sports tests be performed before freeing athletes to play. This includes meeting all criteria based on mobility and strength, as well as specific sporting tests, such as simulated sporting activity, sports practice, playing at a lower level and the player feels ready and confident. In addition, SSC should be considered to play an important role during the late phase of stacking and accelerating launch. Particular attention should therefore be paid to this stage of launch during the specific rehabilitation of sport. A slow reintroduction in sport is also recommended, using irritability as a guide for progression. CONCLUSION The purpose of this clinical commentary was to present a detailed rehabilitation protocol for use after the repair of the SSC. The success of SSC repair depends on the proper rehabilitation, proper surgical technique and examination of other procedures performed. The qualified application of stress to healing tissues guides therapy. This rehabilitation programme advances through five phases with objective criteria requirements to advance to the next phase. Phase I focuses on the protection of passive ROM repair and initiation. Phase II advances on active and assisted ROM as tolerated with an approach to resistance and movement performance without compensation. Phase III progresses muscle strength by incorporating bands, cords, dolls and manual resistance as needed. Phase IV begins to prepare the person to return to the activity or to the occupational demands when dealing with power, agility and speed. Phase V focuses on returning the athlete to pre-injury sports levels. The ultimate goal of rehabilitation is to maximize the patient's ability to return to full ADL, work and recreational activities. The criterion for progression through each phase is based on functional markers and objectives with regard to the time frames for tissue healing. The current review has mixed current literature and expert opinion to report on the development of the rehabilitation guidelines after the repair of the SSC. REFERENCESFormats: Share , 8600 Rockville Pike, Bethesda MD, 20894 USA
Subscapularis Tendon Injuries | Boston Shoulder Institute

Partial rotator cuff tear – Do you really need a surgery? – Caring Medical Florida

Partial rotator cuff tear – Do you really need a surgery? – Caring Medical Florida
ROTATOR CUFF TENDON INJURY, DIAGNOSIS, TREATMENT AND RECOVERY - jointspecialists.org

Subscapularis Repair - Dr. David Duckworth

Partial rotator cuff tear – Do you really need a surgery? – Caring Medical Florida

Tears of the Subscapularis: Hidden and Forgotten, No More! - Shoulder & Elbow
Supraspinatus Tear
Supraspinatus tendon tear: what is it, symptoms, causes, prevention and treatment | Top Doctors
Rotator Cuff Tears: Frequently Asked Questions - OrthoInfo - AAOS
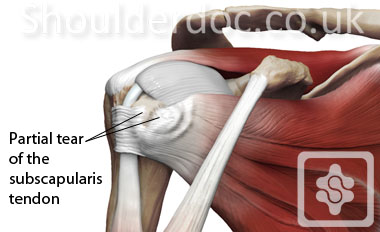
Subscapularis Tendon Tears | ShoulderDoc
Ruptured Rotator Cuff
Subscapularis Tendon Injuries | Boston Shoulder Institute

Subscapularis Repair - Dr. David Duckworth

Treatment options for Failed Rotator Cuff Surgery – Caring Medical Florida

Treatment of Isolated Subscapularis Tears - Cancer Therapy Advisor

Subscapularis tears: hidden and forgotten no more - JSES Open Access
Rotator Cuff Tear - Hobart Orthopaedics
Rotator Cuff Injuries: Symptoms and Treatment - CIO

Subscapularis - Physiopedia
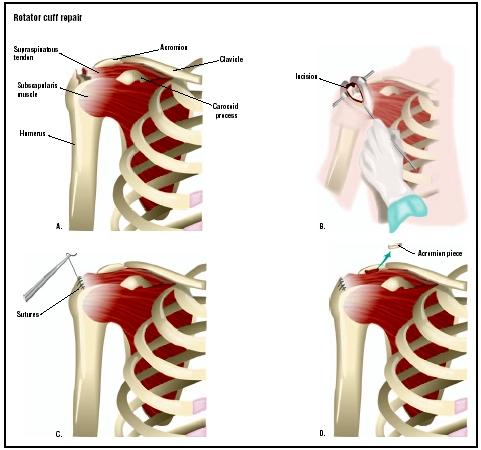
Rotator Cuff Repair - procedure, recovery, blood, pain, complications, time, infection, medication

Subscapularis tears: hidden and forgotten no more - JSES Open Access
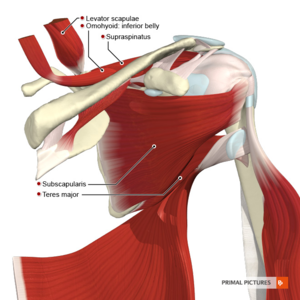
Subscapularis - Physiopedia
Rotator Cuff Repair Chicago | PRP Injection Chicago | Rotator Cuff Doctor Glenview, IL
Causes and treatment for Rotator Cuff Tears

Case Study : Supraspinatus Tendon Tear
Shoulder impingment|Dr Wade Harper Shoulder Surgeon
Rotator Cuff Tear | Symptoms, Repair, & Recovery Time

Rotator Cuff Tear; Rapid Recovery: Paul C. Murphy, MD: Sports Medicine Specialist
Supraspinatus Tear - Symptoms, Causes, Treatment & Rehabilitation

Subscapularis tear: (a) tear of the subscapularis tendon, (b)... | Download Scientific Diagram

Subscapularis Tendon Tears | ShoulderDoc

Rotator Cuff Repair Surgery: Hospitals, Surgeons & Cost | MedcureIndia

Subscapularis Tear: Symptoms, Treatments, Recovery
Rotator Cuff Tear Settlements (Car Accidents, Motorcycle Accidents, Etc.)

The procedure for subscapularis tendon repair. (A) 3.7 mm punch for a... | Download Scientific Diagram
Shoulder impingment|Dr Wade Harper Shoulder Surgeon
Rotator Cuff Tears - OrthoInfo - AAOS
Can A Torn Rotator Cuff Heal On Its Own Without Surgery?

Subscapularis Tear: Symptoms, Treatments, Recovery
Posting Komentar untuk "subscapularis tendon tear recovery time"